

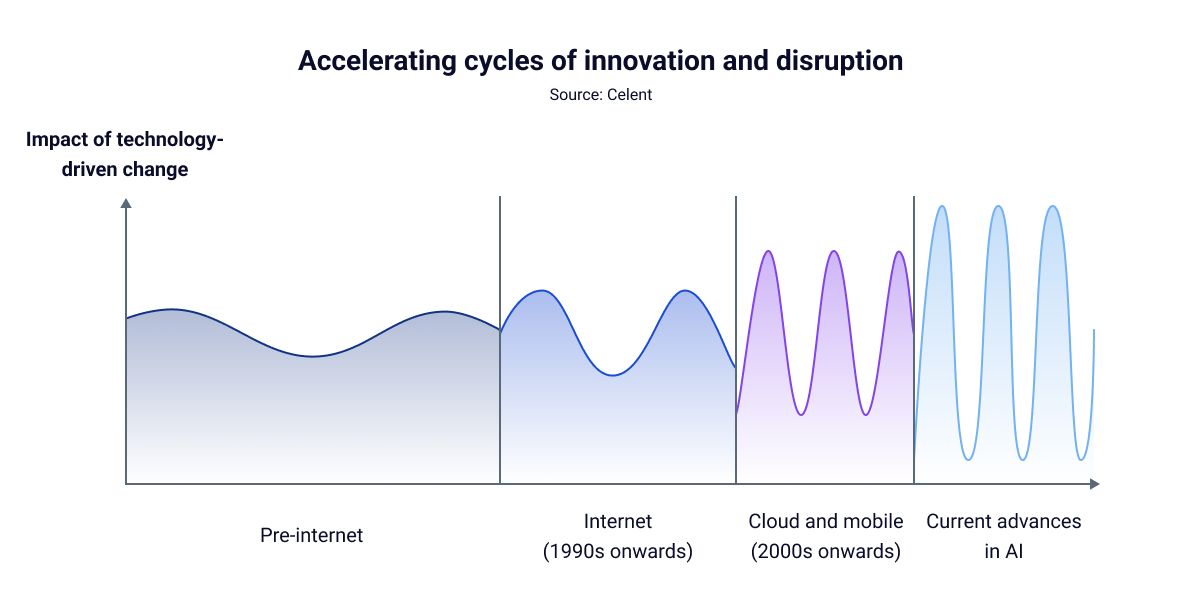
The landscape of innovation in P&C insurance is changing fast. It’s not just that new technology is available to carriers, the cycles of innovation themselves are speeding up. What used to be moderate, gradual change has accelerated to a breakneck pace with the latest advances in AI.
This is uncharted territory for carriers. Falling behind is no longer an option, and waiting on the sidelines isn’t either. The pace of change is simply too fast.
This blog will cover some of the key shifts in AI for P&C insurance and share five keys to adopting AI successfully while keeping up with the rapid pace of change.
The pace of change is staggering, and the demand for AI use keeps climbing. ChatGPT alone now handles more than 2.5 billion daily requests, according to OpenAI. That surge shows how quickly user expectations are shifting, with more people wanting customizable solutions at their fingertips. Agentic AI is also on the rise and is expected to materially reshape the workforce in the coming months and years.
As the conversations carriers are having about AI shifts from understanding to implementation, generative AI is seen as having the highest immediate impact, while agentic AI is expected to drive the biggest changes in the near term. Looking further ahead, carriers also rank quantum computing and artificial general intelligence as high-impact technologies, according to recent research by Celent.
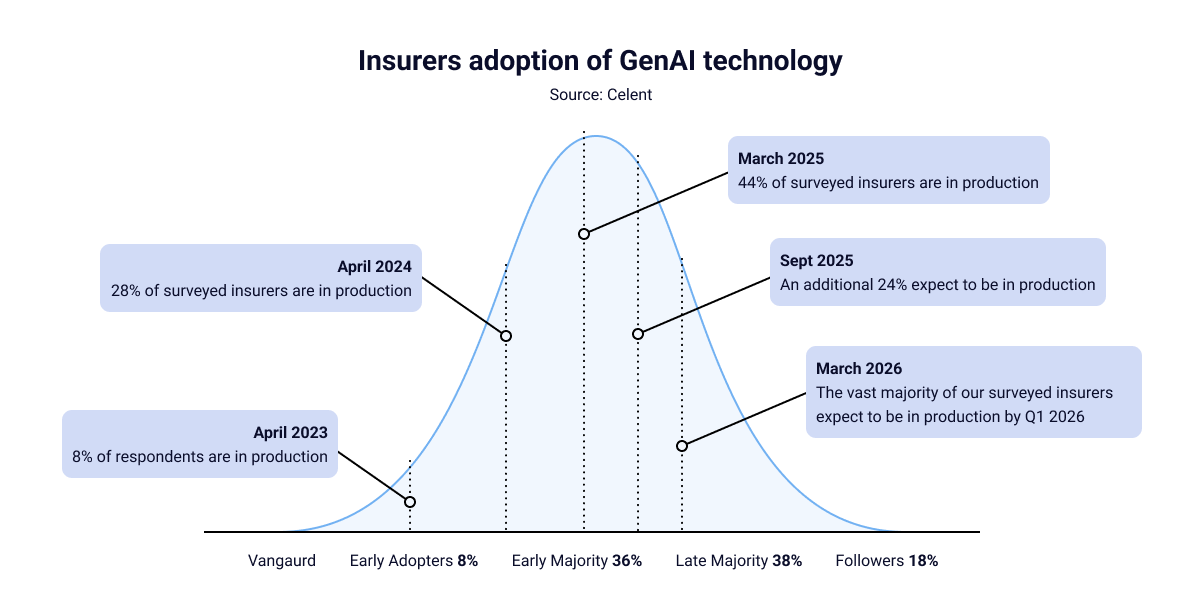
One notable recent change is the increasingly positive sentiment toward GenAI adoption, reflected in rising adoption rates. According to Celent’s 2025 Insurance GenAI Adoption survey, 44% of respondents are already in production, with another 24% expected to move into production within the next six months. Among those with AI in production, 88% are focused on employee use cases—up sharply from 20% in 2024. This shift shows that attitudes are changing, with both employees and employers embracing these technologies for their benefits.
Likely contributing to the increased adoption of GenAI in insurance is the ROI already being realized by carriers. In Celent’s insurer survey, nearly one-third (32%) of respondents reported greater efficiency from GenAI, 29% reported higher productivity, and 9% reported reduced costs.
While implementing new technology can be time-consuming and results aren’t always immediate, these early returns highlight the long-term impact GenAI can deliver and the efficiencies still to be gained.
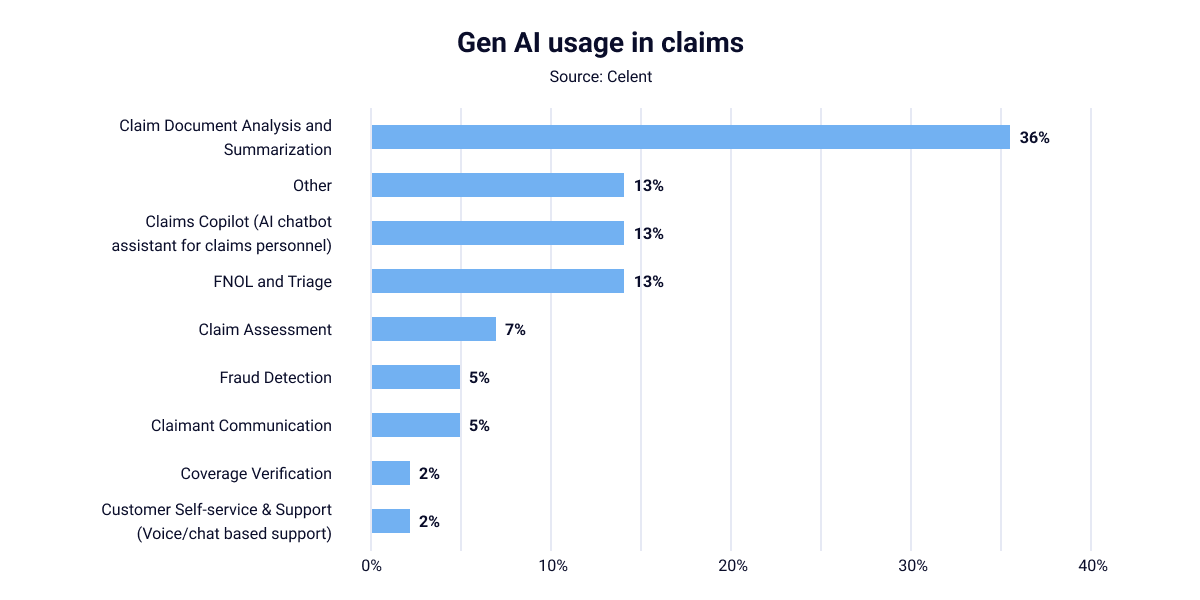
In claims, GenAI is most commonly used for document analysis and summarization. Solutions like DigitalOwl’s AI for medical record reviews are being adopted to increase efficiency, improve accuracy, and enhance the quality of data analysis.
Other use cases include AI chatbots, first notice of loss (FNOL), and triage at 13%, while claim assessment, fraud detection, and claimant communication represent a smaller share of GenAI adoption in claims.
P&C carriers are under pressure like never before. Case volumes are rising, medical records are more complex, and policyholders expect faster outcomes. At the same time, 58% of carriers say claims will be the area most impacted by AI in the next two years.
Yet despite the clear ROI already being seen, adoption hesitancy remains. Concerns about compliance, governance, and organizational readiness are still top of mind. The good news is, we know what separates successful adopters from those who stall.
Recent survey data highlights the most important factors for realizing the benefits of GenAI. Here are five key elements claims leaders should focus on.
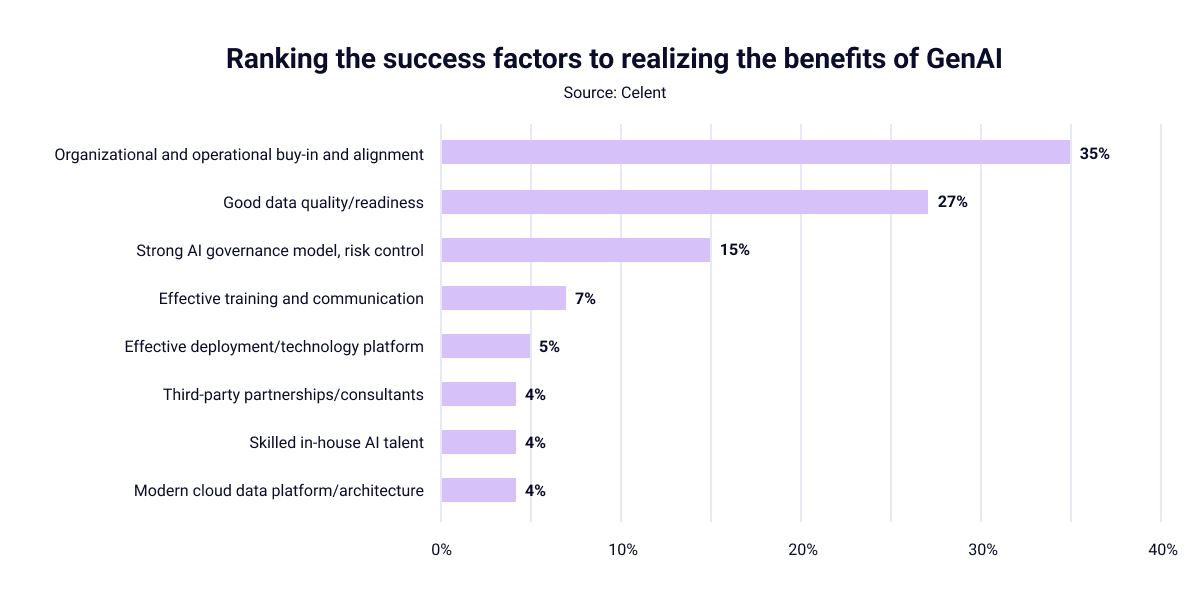
The number one factor, cited by 35% of respondents, is organizational and operational buy-in. AI can’t be adopted in a siloed environment. It requires alignment between leadership, IT, compliance teams, and claims adjusters.
Here are some practical steps for ensuring organizational buy-in:
AI is only as good as the data it’s trained on. Nearly one-third (27%) of respondents ranked good data quality as the top success factor in implementing AI in insurance. Poorly structured or incomplete claims data can undermine even the most advanced AI solutions.
Consider the following steps to improve data quality before implementing AI solutions:
Another 15% of respondents identified governance and risk control as the top requirement for AI implementation. This process is critical. Without clear oversight, carriers risk missteps in compliance, ethics or explainability that could get them into hot water with regulators.
Here are some tips for building strong AI governance:
Only 7% of respondents ranked training as their number one factor for success, but it’s often the difference between organizational adoption and abandonment during the POC. Even the best technology will fail if your team doesn’t know how to use it.
For this reason, it’s important to consider the following steps:
Technology deployment, third-party expertise, and cloud platforms ranked lower individually (5% each or less)—but combined, they play a critical role in scaling adoption. Skilled in-house talent and trusted external partners accelerate time-to-value.
Here are some key steps for finding the right partners:
DigitalOwl helps claims teams improve the efficiency, quality, and accuracy of medical records by transforming unstructured data into organized, reliable insights, summaries, and timelines. To learn more about how we can help you adapt to the future of claims, contact us today.