

The current landscape of P&C claims is complex, demanding, and high stakes. Claims professionals are at the core, where a high level of expertise is required for negligence and coverage determination, record analysis, evaluation and negotiation, and understanding jurisdictional impact.
Multiple technologies and vendor solutions have been introduced to ease the burden, but challenges tied to the required expertise and demanding nature of the work remain. As a result, the industry remains weighed down by inconsistent outcomes, and valuable time spent on manual tasks like medical record reviews.
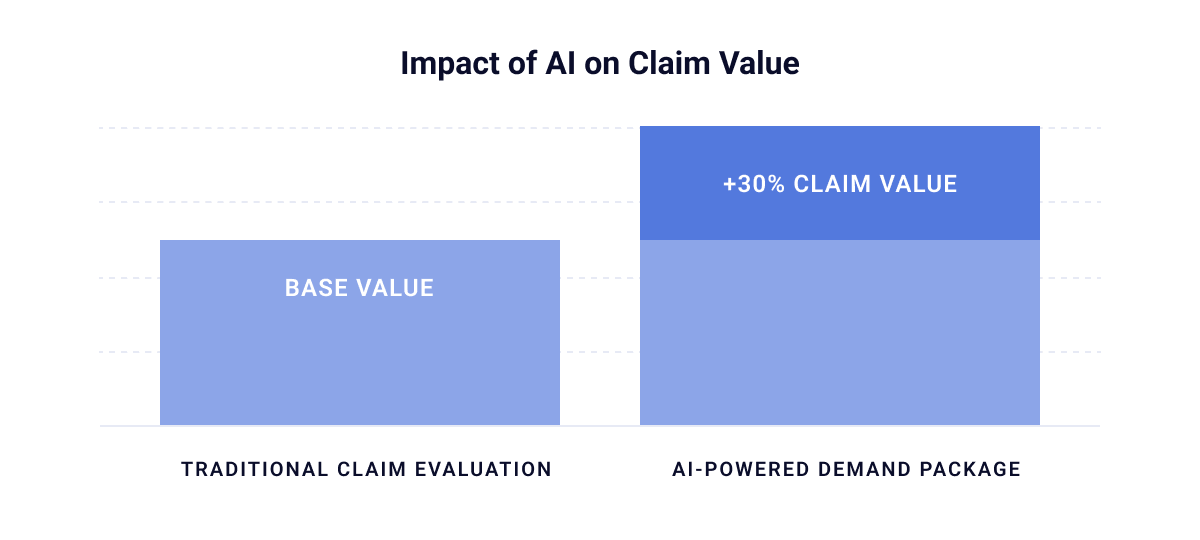
On the other hand, plaintiff attorneys have quickly adapted to technological advancements, and are using artificial intelligence (AI) and other tools to generate robust demands almost instantly and drive up the value of injury claims. Some AI-powered demand package companies even claim they can increase claim values by as much as 30%.
This can overwhelm claims professionals, whose open caseloads typically range from 100–150 claims, with some approaching 300. This contributes to the inconsistency in how injuries are assessed, leading to suboptimal outcomes and leakage. In fact, a 2024 analysis by WorkCompCollege found that high caseloads and inconsistent file workups can drive claim costs as much as 20% higher, due to errors like the failure to control expenses, missed subrogation, and poor investigations.
To move past these challenges, P&C carriers must make a shift toward solutions that reduce variability and unlock enterprise-wide improvements in efficiency, quality, and accuracy.
The rise of AI and GenAI solutions has opened a new frontier in claims management, delivering improvements in consistency, accuracy, quality, and speed. AI-driven medical record summaries and data analysis are leading this transformation, enabling organizations to implement strategies that scale effectively and deliver sustainable performance gains.
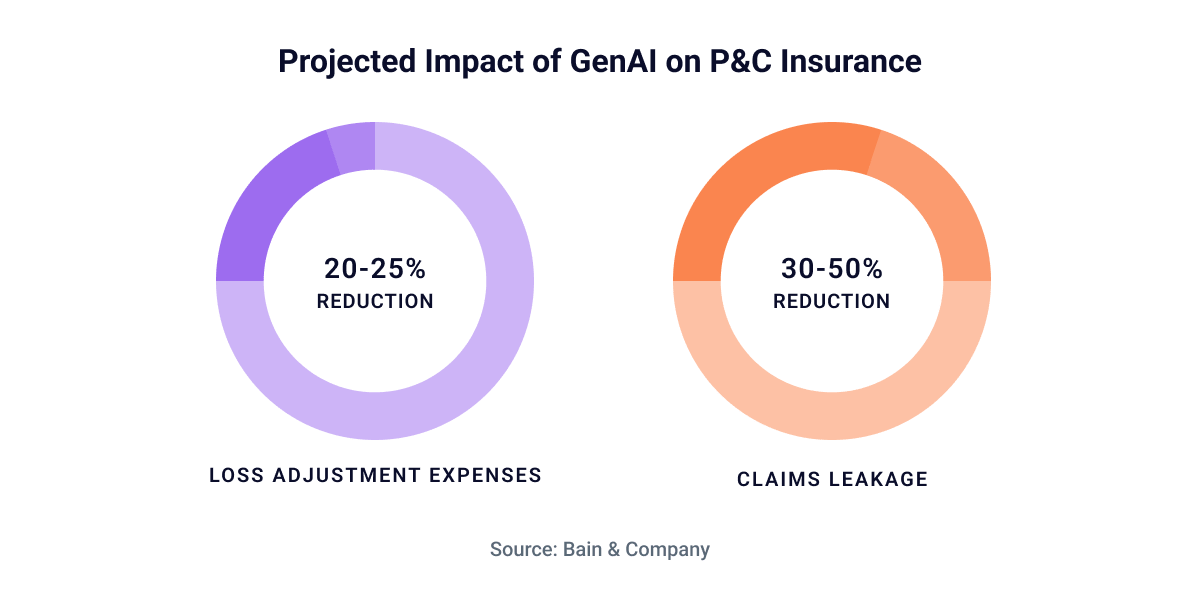
These strategies are fueled by key value drivers, which will have a major impact on organizations’ bottom lines. Industry research underscores this point, with analysts at Bain & Company predicting that Gen AI could reduce loss adjustment expenses by 20% to 25% and cut claims leakage by 30% to 50% in P&C insurance alone.
The value realization is seen at an organizational level. It’s now possible for claims professionals to review and analyze the full set of medical data and facts so that nothing is overlooked, while also sharpening focus on the information that directly impacts evaluation and value determination. It brings standardization to the evaluation phase, reducing discrepancies across adjusters, and frees up time for professionals to concentrate on developing the critical skills of evaluation and negotiation, which are the competencies separating top performers from the rest.
The most impactful value extends beyond efficiency. Experience gaps are minimized as technology elevates more adjusters to perform at the level of the very best. Leakage and errors decline rapidly, directly improving indemnity results. Accuracy and quality rise to consistently high levels, while evaluation and decision-making accelerates, limiting the influence of attorneys and litigation that drive up costs. At the same time, capacity is created for peer reviews and roundtable discussions, expanding opportunities to refine strategies and drive optimal outcomes across more files.